Eating disorders like not eating enough or eating too much and then getting rid of it can significantly impact several aspects of health, including oral health. These disorders often involve restrictive eating patterns or purging behaviours, leading to nutrient deficiencies that can significantly impact oral health. Calcium, a crucial component of enamel, is often lacking in eating disorder patients, increasing the risk of dental erosion, tooth decay, and tooth sensitivity.
Being ignorant of these disorders and their damaging impacts on dental health will lead to the development of severe diseases and expensive treatments. Let’s familiarise you with these disorders and the need for early identification to prevent irreparable damage to teeth and gums.
Specifics of Eating Disorders
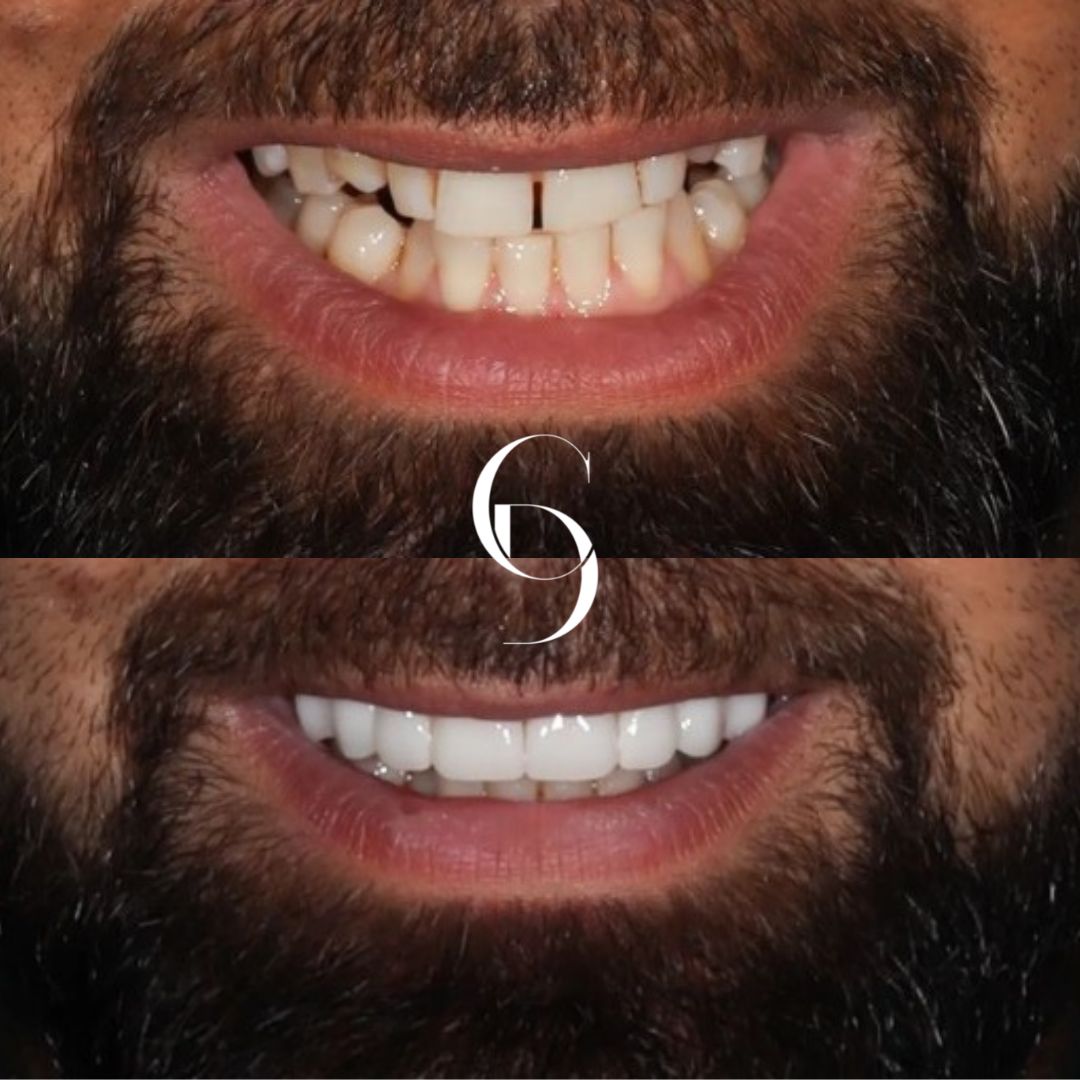
Some of the most frequent eating disorders that damage your teeth and lead to treatments such as dental implants, dental root canals, fillings, crowns, dental veneers, and others.
Bulimia Nervosa
This disorder includes a fear of being overweight as well as periods of hidden binge eating. These episodes can happen several times per week or even several times per day.
When someone binge eats, they lose control and eat a lot of food, commonly high in fats and carbohydrates. Following a binge eating episode, someone suffering from Bulimia will frequently attempt to purge the food by forced vomiting, the use of laxatives or enemas, fasting, or extreme exercise. Overeating and forced release are referred to as bingeing and purging.
Binge Eating Disorder
Binge eating disorder, like Bulimia, involves consuming large amounts of food in a short period. The distinction between BED and Bulimia is that those with BED usually experience emotions of guilt and humiliation after binge eating, whereas those with Bulimia try to get rid of the binged food by using laxatives or vomiting.
The Impact of Eating Disorders on the Mouth and Teeth
Swollen Salivary Glands: The salivary glands can swell due to a binge-purge cycle. A regular binge-and-purge cycle can promote salivary gland hypertrophy. Overeating, particularly sugary or acidic foods, can overload the salivary glands, causing them to overproduce saliva and become swollen. The excessive acid from these foods can also irritate the salivary glands, further contributing to inflammation. Enlarged glands can be painful and are frequently visible to others, causing emotional distress.
Chronic Dry Mouth: Our mouth experiences decreased salivary flow due to dietary deficiencies, bingeing, and purging. A dry mouth causes a range of uncomfortable symptoms, such as a dry, sticky feeling in the mouth, difficulty swallowing, and impaired taste sensation. This makes the mouth extremely dry due to dehydration, causing lips to become reddened, dry, and cracked.
Tooth Decay and Gum Disease: Since calcium and vitamin D are essential for maintaining oral health, insufficient amounts of these minerals can increase the risk of gum disease and tooth decay. Food restriction often results in nutritional deficiencies. Calcium, iron, and vitamins B are all nutrients that enhance oral health. Inadequate calcium promotes tooth decay and gum disease. Too much brushing of teeth following a purging session could further worsen dental decay.
Bad Breath: Overeating can lead to excessive food particles remaining in the mouth, particularly between teeth and on the tongue. These food particles create a breeding ground for bacteria that produce volatile sulphur compounds (VSCs), the main culprits behind bad breath. Additionally, Purging, a common behaviour in eating disorders, can cause stomach acid to reflux into the mouth. This stomach acid can coat the tongue and other oral tissues, creating a favourable environment for bacteria and contributing to bad breath.
Tooth Sensitivity: Regular vomiting allows stomach acid to run over the teeth, causing the enamel (outer layer) to erode. This could end up in hot and cold sensitivity, discolouration, and weakened/brittle teeth.
Jaw Arthritis: Degenerative arthritis of the temporomandibular joint in the jaw is a dental problem that is frequently linked to eating disorders. This is the joint that connects the lower jaw to the skull. When arthritis develops in this joint, it can cause joint discomfort, recurrent headaches, and difficulty eating and opening/closing the mouth.
The Verdict
It is critical to seek treatment if you think you have an eating disorder. Dentists can educate you on how to better care for your teeth, preventing the development of dental-related disorders.
Your dental doctors can refer you to treatment choices depending on the type of eating disorder. They specialise in dental X-rays, porcelain teeth, broken tooth repair, veneer teeth, and dentures, among other things. They will easily determine the best method for your teeth.